Nar(can) Save Lives: It's worth the Cost
Tim Gear, a first-year student at American University, knows the dangers of heroin. His father was a heroin addict who overdosed several years ago and owes his life to Narcan, an overdose reversal agent.
“I know a lot of my dad’s friends who also were saved because of Narcan, and since they got that second chance they have gone on to live a clean and sober life,” Gear said. “If it wasn’t for the administration of Narcan, then I wouldn’t be here.”
Gear’s dad was almost one of nearly 13,000 Americans in 2016 who died from heroin overdoses, according to the American Society of Addiction Medicine.
According to the Centers for Disease Control (CDC), heroin use has doubled within the last decade and heroin-related deaths have tripled. The use of heroin and other opioids is not concentrated to any single socioeconomic group.
While policy makers are having conversations about how many people are dying, who is being affected and how the nation is suffering, they are remaining silent on Narcan. And when they do talk about Narcan, the conversation is focused on the cost.
Benjamin Miles, a Board Certified Pharmacotherapy Specialist who holds a doctorate in Pharmacy, works in the Emergency Department at Sibley Hospital. He has seen a steady increase in the number of overdoses in the last seven years.
Though some say Narcan enables addiction by providing a safety net for addicts, he argues that there should be more public funding for Narcan distribution.
“Narcan is important because it’s the only way to treat an overdose,” Miles said. “What enables the addiction, a lot of the time, is overprescribing of opioids.”
Narcan, also known as naloxone, has been produced since 1971. It was originally used in hospitals to prevent overdoses on prescription opioids like morphine. In recent years, Narcan’s use has shifted: It has passed from the hand of doctors to the general public.
According to a 2015 CDC report, opioid overdoses can be reversed if Narcan is administered immediately. While first responders are often successful in reviving an overdose victim, sometimes they arrive too late. If family members and friends had Narcan and knew how to administer it, more overdoses could be reversed.
Last September, D.C. lawmakers passed a bill to allow pharmacists and physicians to prescribe Narcan to those at risk of overdosing and permitted community based organizations to dispense it, according to the Washington City Paper. This law also protects medical professionals from legal ramifications when dispensing Narcan.
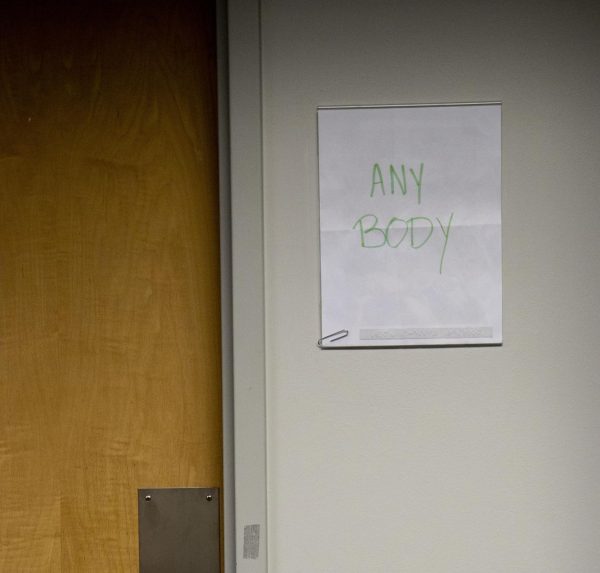
Several organizations, like Helping Individual Prostitutes Survive (HIPS), support the supplying of Narcan kits. HIPS gives free Narcan kits to anyone who requests one. When the CDC launched a pilot program in D.C., using federal funding to purchase and distribute Narcan to nonprofits in the area, HIPS participated in this pilot program. The organization receives Narcan kits from the government.
All HIPS staff and volunteers are trained to administer Narcan, and can train others. Confidential workshops are available to the public during their office hours.
“Anyone can come in at any time to get Narcan,” said a HIPS volunteer who wished to remain anonymous because they had received services from the organization. “All you have to do is a quick course in a private room where we use a tester kit to show how to administer the drug, and then you can sign off to receive a kit for free.”
As the debate over the public and private costs of healthcare rages across the country, conversations about Narcan are mostly centered around the cost. Narcan kits can cost up to $50, but reversing an overdose often requires multiple kits.
In order to purchase these kits, first responders in D.C. have access to hundreds of thousands of dollars in public funds. Private citizens, however, typically pay out-of-pocket. Further, Miles says that when overdose patients can’t pay their hospital bill, the hospital ends up losing money and resources. Sibley writes unpaid overdose bills into its budget.
While pharmacies do offer Narcan, it can only be purchased with a prescription from a doctor in most states, and is rarely covered by insurance companies. Medicaid, a government insurance company that provides healthcare coverage for low-income people, covers the medication in certain states.
Despite multiple attempts to reach out to Public Safety for a comment, their officers were not able to speak on the record about AUs policy on drug overdoses and the use of Narcan. It is not known at this time whether Narcan is purchased or carried by the school. If it is not available to Public Safety officers, there could be additional lag time between the discovery of an overdosed student and Narcan being provided, which could cost student lives.
Gear hopes the uncertainty over Public Safety’s ability to use Narcan will be addressed.
“Narcan can save lives and I hope that if it [an overdose] happened on campus, someone would be able to act fast enough to save [the] student,” Gear said.
It’s difficult to quantify the cost of human life, but making Narcan accessible to the public is a move that could save both money and lives—a hospital visit is almost certainly more expensive than a Narcan kit.
Ultimately, the question is, on whom the burden of paying for Narcan should fall: the taxpayers, or patients and their families, who may be unable to afford it. After all, an addict can’t get clean if they aren’t alive.
“It’s only fair to give them a second chance,” Gear said.

I'm a Senior majoring in Journalism, interested in science, drug policy, homelessness, crime and punishment, and philosophy.
I emerged from the woods...